IMPORTANT: Medicare does NOT accept corrected claims. Instead of following the instructions below, make the necessary changes and resubmit the claim without any Corrected Claim Indicator. Medicare won't reject the claim for being a duplicate, but they will reject the claim if it includes the Corrected Claim Indicator.
Jump to Section:
When a claim is rejected or denied for incorrect information, often times the payer will require you to resubmit the claim with both the necessary changes and a Corrected Claim Indicator. There are multiple indicators with different meanings:
- 1 = Original Claim Submission
- 7 = Corrected/Replacement Claim
- 8 = Void Claim
The system is able to send these claims, however you will need to follow a few steps in order for our system to make the necessary changes.
ICN or Payer Control Number
- The first step is to find the ICN, if the claim was denied, or the Payer Control Number if the claim was rejected. The ICN is found on your EOB, located under the Deduct column.
- If you did not receive an EOB for the claim, meaning it was rejected, then you can search for the Payer Control Number in the Claim Status Tab. For help understanding how to find that tab, click here.
-
Once you've found the claim, click anywhere on the claim line, and it will drop-down with information. To the far right of the line, located underneath the Action button, there is a column called Payer Control Number.
-
Edit the Claim: Box 22
Once you have either the ICN or Payer Control Number, click the drop-down in box 22 to select Original, Corrected or Void. Then enter the ICN or Payer Control Number in box 22 under the original reference number.
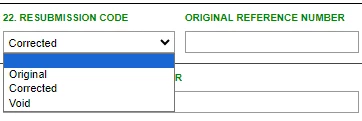
This will notify the payer which claim is being replaced in their system so that they don't mark the claim as a duplicate.
NOTE: You CANNOT submit a corrected claim without an ICN or Payer Control Number. Insurance companies will reject claims if they are sent with a corrected/replacement indicator, but no claim to associate with the replacement. The same goes for sending a claim with an ICN/Payer Control Number, but not including the corrected claim indicator.
Once you have made the changes, click the Resubmit Claim button, and it will be sent to the payer.