Prerequisites
The Acorn script includes all billing requirements EXCEPT:
- A SubProgram Service component must be configured and populated with all appropriate SubPrograms.
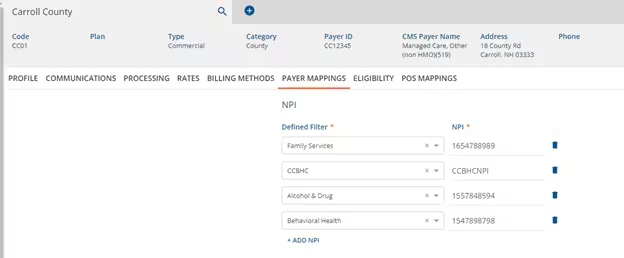
- A Defined Filter should be created for CCBHC services. This Defined Filter must be saved against the agency’s CCBHC-specific NPI in Payers > Payer Mappings for all Payers who apply.
- Once the SubProgram is configured, the id of that component must be placed into the following script in place of ‘the ‘x’ and run: INSERT INTO StaticValues(PropertyKey, PropertyValue) VALUES('SUBPROGRAM_COMPONENT_ID', 'x')
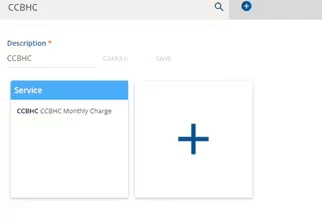
Service Definitions Required
- A CCBHC PPS 2 “T1041” service definition for each Acuity level.
- Set as a Per diem Service type
- Only include a new unique Activity Component value for each Service Definition.
- Set Rate as “Not billable to most payers.”
- Add Rates and Modifiers for the Medicaid payers
- TPL Indicator Service “S9986”
- Default Service Type
- Only include a new unique Activity Component value
- Set Rate as “Not billable to most payers”
- Add a Base and Contracted Rate of .01 for Medicaid payers
All other services required are those your agency provides, whether CCBHC-eligible or not.
Forms
All forms loaded by the Acorn are installed under Forms.
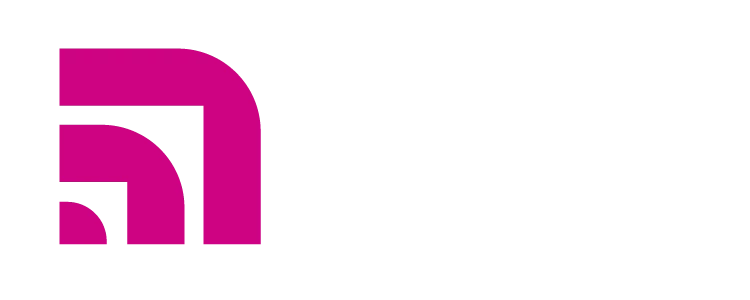
CCBHC Eligible Services
- Enter all Services that should be reported as shadow claims when reporting billing the PPS2 service.
- Enter Y Yes in the Qualifying field if having the Service would qualify the Client to receive the PPS2 rate for the month.
- Under S9986 Service, enter Y Yes only for the TPL Indicator Service.
- The Start Date and End Date fields are optional.
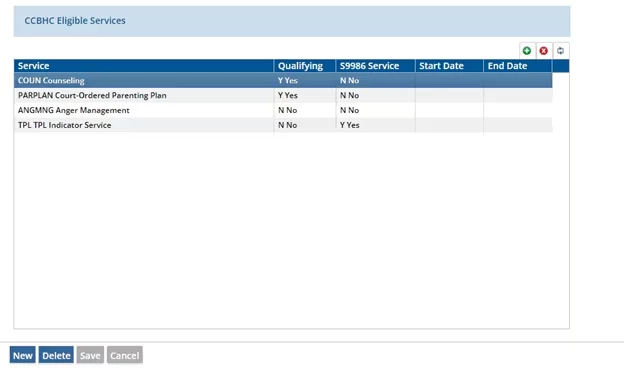
CCBHC Payers
- Enter the Payers that may be billed the CCBHC PPS2 Rate.
- The Start Date and End Date fields are optional.
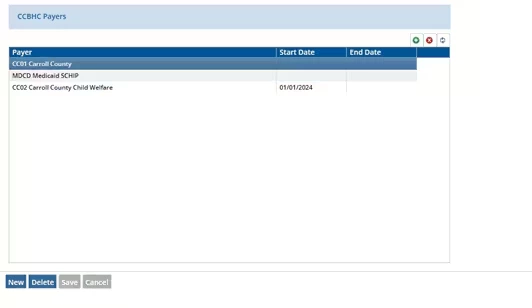
Excluded Locations
Enter any Service Locations that exclude a service from CCBHC eligibility.
CCBHC Program Mappings
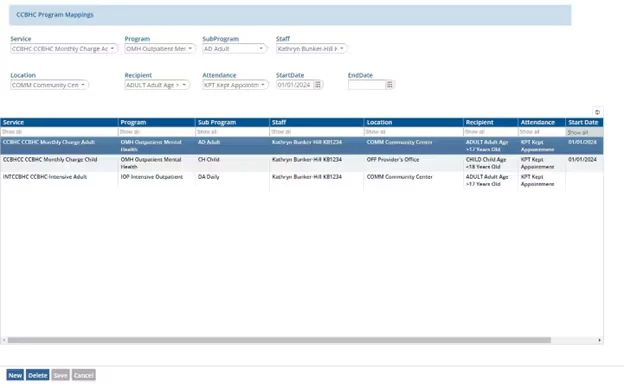
- Map your Enrollment Program/Sub Program combinations to the correct CCBHC PPS2 Service Definition.
- Enter the Staff that should be reported for that CCBHC PPS2 Service.
- Enter the Location, Recipient, and Attendance code that should be used on the PPS2 Services.
- The Start Date and End Date fields are optional.
Creating the Monthly CCBHC Services
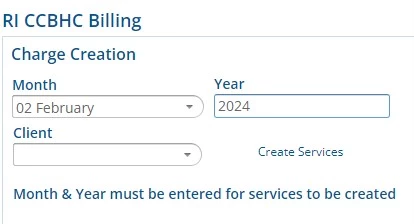
- To create the PPS2 Services, enter values into the Month and Year fields.
- Click Create Services.
PPS2 (T1041) and TPL Indicator (S9986) Services are created as follows:
PPS2 Services:
- One monthly CCBHC service (T1041) for each Client for the Enrollment with a Program/Sub Program that matches an Acuity Level Service Definition AND for which the Client received a qualifying service (in ready, charge created or done status) at an approved Location (not in the Excluded Locations).
- The Enrollment Dates must include the month being billed.
- Services are only created for Clients with an Active Client Payer at time of service that is included in the CCBHC-Eligible Payer list.
- The Service created will have a Start Date of the first day of the month and an End Date of the last day of the month, except when:
- The client enrollment started within the month, and in that case, the Start Date will be the first date of service.
- The client enrollment ended within the month, and in that case, the End Date will be the enrollment discharge date.
- The client payer eligibility started within the month, and in that case, the Start Date will be the first date of payer eligibility.
- The client payer eligibility ended within the month, and in that case, the End Date will be the payer eligibility end date.
- The Service Definition for the Service will match the Program/Sub Program mapping.
- If a Monthly CCBHC Service has been created for a given Client for a given month, another will not be created.
S9986 TPL-Indicator Services:
- If a Client has had a charge created for a CCBHC-eligible Service that is now in an Active status (Active, Outgoing, Working, Denied, Done) to a Primary Payer, the process will create one shadow service (S9986) to indicate that Claims are pending TPL adjudication within the period being billed.
- The date of service will be the date of the first Service of the month OR the date of the Client’s first Service if the Enrollment is new.
- Units for this service will be ‘1’.
- Services created are set to Not Ready Status, so they can be reviewed, edited, or deleted prior to billing.
- Diagnoses for these Services are pulled from the Clients’ Primary Diagnosis unless missing in which case we will pull from the last shadow claim of the month.
Services may be Marked Ready and processed through Unprocessed Services.
837 Billing
The 837 Acorn must be selected in the 837P Billing Method for all appropriate Payers:
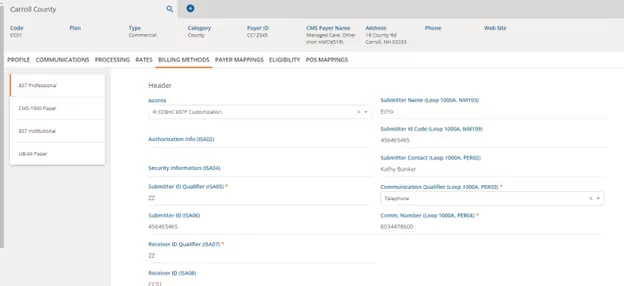
Other Configuration Required:
- Create a CCBHC Defined Filter that can be used to assign to the CCBHC NPI
- Create a Non-CCBHC Defined Filter that can be used to run Non-CCBHC claims through Unbilled Charges.
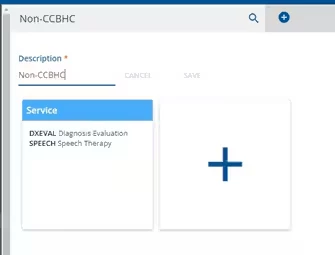
Bills may be run at any time during the month for Non-CCBHC Services.
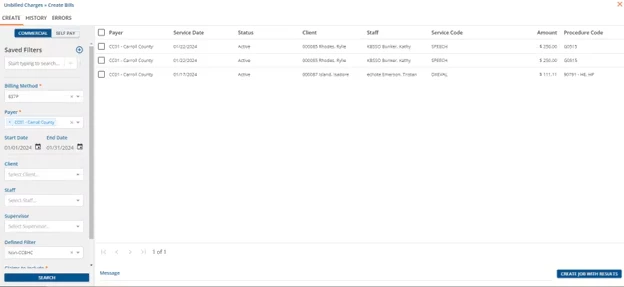
At the end of the month, after running bills for all Non-CCBHC Services, run Claims for the CCBHC Claims.