PERMISSIONS REQUIRED: Supervisees must have Notes require supervisory review enabled with supervisory setting of Must review and approve all notes OR Must review and co-sign all notes.
After the assigned Staff Member has reviewed and approved your Initial Assessment, Treatment Plan or Progress Note you will receive an email and alert notifying you that you can now either sign or co-sign the Initial Assessment, Treatment Plan or Progress Note. Once your supervisor has approved or co-signed your document, you can then apply your signature.
NOTE: You can prevent your staff from submitting and signing progress notes that do not have a diagnosis code entered. See Prevent Staff from Submitting/Signing Progress Note without a Diagnosis for more information.
- The supervisor approves the Initial Assessment, Treatment Plan or Progress Note.
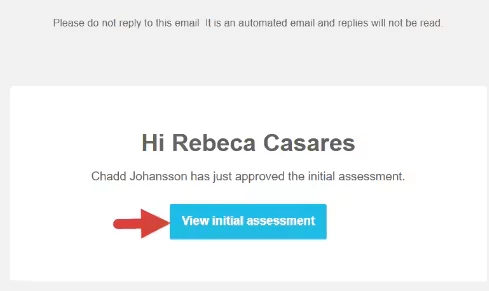
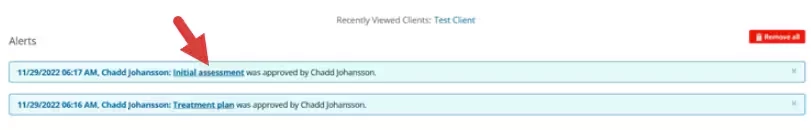
- The supervisee receives an email and alert notification to let them know an Initial Assessment, Treatment Plan or Progress Note has been approved.
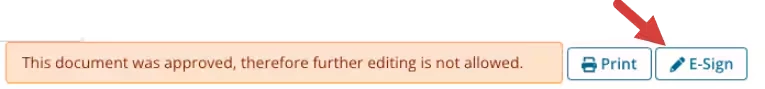
NOTE: No changes can be made to the document after it is approved. A message displays when the supervisee views the document:
This document was approved, therefore further editing is not allowed.The supervisee can still E-sign the document even though it has not been signed by the supervisor. Learn more.
- Review the approved document from the email or alert page.
Email
Alert page
- Review the approved document from the email or alert page.
- Click E-Sign. Learn more.
- Click Sign the Document button in the Document Info section.